Point Mutations and Reassortment
The genetic code of viruses can consist of DNA or RNA. Influenza viruses have RNA. This code has an alphabet of four different letters called nucleotides, namely adenine (A), guanine (G), cytosine (C), and uracil (U). A sequence of three of those letters defines the amino acid to be built. A change of one of those letters is a point mutation, which may or may not change an amino acid, since there are 64 possible combinations resulting in 20 different amino acids. However, only changes of amino acids have an impact on how the virus functions.
Influenza viruses have eight separate RNA segments, each encoding different viral proteins. During a co-infection of a host cell with two or more influenza viruses, reassortment can occur. Reassortment means that segments of different viruses mix and match, leading to the production of new viruses with novel combinations of RNA segments. Reassortment events are relatively rare but can have significant consequences. This is why influenza viruses as a whole are dangerous, not just H5N1. With widespread "seasonal flu" infections, every H5N1 infection comes with the risk of H5N1 obtaining all the needed adaptions to mammals in just one reassortment event.
A large number of known mutations can be found on the CDC website. While this may look straightforward, it is important to keep in mind that amino acids are physical objects and not just some kind of computer code. The physical interactions between them can in some cases alter the properties of the virus.
The Focus of Attention: Segments PB2 and HA
The eight segments are PB2, PB1, PA, NP, HA, NA, M, and NS.
PB2 controls a process called polymerase, which is essential for replication in host cells. HA and NA form the surface proteins, that we use for naming the virus subtypes like H5N1 or H7N9. HA (short for hemagglutinin) is responsible for binding the virus to the cell that is being infected. The main challenge for H5N1 are the different sialic acid (SA) receptors in birds and mammals. The various PB2 mutations develop fairly often after infection of a mammal, but there may be an increasing number of those mutations circulating in birds and the food supply, as the double mutation PB2-E627K/PB2-K526R in all Polish cats probably infected by cat food suggests. However, a relevant PB2 mutation has been detected very rarely in birds so far.
Additionally, a PB2 mutation has been found to inhibit the innate immune response.
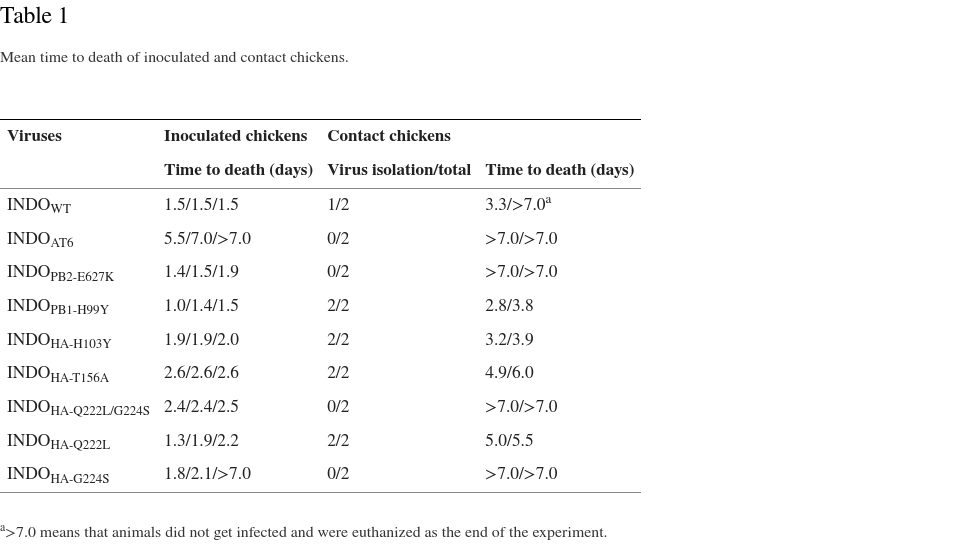
Gain-of-function Experiments and Airborne Transmission
The famous -and controversial- gain-of-function experiment of Ron Fouchier with ferrets, that resulted in airborne virus transmission, required one PB2 mutation and three HA mutations. Currently the PB2 mutation and one of the HA mutations are fairly common. In an oversimplified model, that transfers results from ferrets directly to humans, we may be two HA mutations away from a pandemic. There is also the gain-of-function experiment of Yoshihiro Kawaoka, which achieved airborne virus transmission between ferrets. This study used a HA segment from H5N1 with four mutations and replaced the other seven segments with H1N1 segments, simulating reassortment. Another experiment has been conducted with chickens and all mutations required for airborne mammal-to-mammal transmission.
Just One Mutation?
While the gain-of-function experiment of Ron Fouchier et al is a popular reference, there is also a very concerning study about the 1918 H1N1 pandemic virus. It shows that just one mutation can enable the virus to change the sialic acid receptor binding specifity from birds to both birds and mammals. Such a mutation in H5N1 would drastically increase the chances of a pandemic, although further mutations would still be required.
And recently a dangerous mutation which increases the sialic acid receptor binding specifity to mammals, even without reducing the preference for birds significantly, has been discovered in birds.
In this study, we confirmed the ability of the rCT/W811-HA193D to replicate efficiently in ferrets and human bronchial epithelial (HBE) cells, showing replication efficiency similar to that of the 2009 pandemic CA/04 H1N1 influenza virus, suggesting that these viruses pose a potential threat to human infection.
Natural Bird Flu Defenses
A very recent study has discovered human BTN3A3 (butyrophilin subfamily 3 member A3) as a potent inhibitor of avian influenza. However, a mutation in the NP segment, NP-313F, enables evasion of this mechanism and seems to be fairly common.
This is not to be confused with the basic virus defense mechanism regulated by Mx1, which is not limited to humans, and where genetic improvements made mice resistant to influenza A viruses.
A unique feature of the NS segment of H5N1, NS-92E, confers resistance to interferons and tumor necrosis factor α, basic defense mechanisms against all kinds of threats. Not only may this contribute to the high case fatality rate of H5N1, but it has been proven that other influenza viruses can become more dangerous should they acquire the H5N1 NS segment in a reassortment event.
Vaccination against seasonal influenza (H1N1/H3N2) had increased the antibody response against H5N1 only by a tiny amount. Antibody response to NA of the 2009 pandemic H1N1 virus however correlates strongly with an antibody response to NA of H5N1. This is due to a higher similarity of the NA segments. It is unknown how much actual protection this confers.
Two NA Receptor Binding Mutations
It seems that the receptor binding mutations in HA require mutations in NA like NA-I396M and NA-S369I to reestablish some kind of equilibrium. The NA mutations disrupt the second sialic acid-binding site of influenza A virus neuraminidase, 2SBS, which preferentially binds to α2,3-linked sialic acid receptors most common in birds. This host range determinant has a prevalence of 3% of the H5N1 A/Herring_gull/France/22P015977/2022-like genotype.
In addition to the distinction between alpha 2,3-linked sialic acid receptors and alpha 2,6-linked sialic acid receptors, there are Neu5AC and Neu5Gc sialic acids. However, humans share Neu5AC sialic acids with susceptible species like ferrets and seals.
Amantadine and Rimantadine
Due to widespread resistance mutations in the M segment, mostly M2-S31N/L26I, the M2 inhibitors amantadine and rimantadine are no longer used. However, scientists try to find ways to inhibit the resistances to the inhibitors - an arms race between scientists and the virus.
Other Resistance Mutations
Mutations of concern are NA-H275Y and NA-I223R. NA-H275Y offers resistance to oseltamivir(Tamiflu), while NA-I223R offers resistance to zanamivir(Relenza). As this study shows, they can emerge quickly under favorable conditions, like prolonged infections in immunocompromised patients. Both mutations amplify each other. While peramivir gets often mentioned in that context, this study indicates therapeutic success despite the NA-H275Y mutation. However, this study reports a highly reduced susceptibility, although 3 to 4 times less reduced than against oseltamivir.
In 2007/2008, when a H1N1 was a significant seasonal influenza strain, H1N1 surprisingly acquired increased resistance to oseltamivir a due to HA-H275Y to a high degree and worldwide. This situation subsided with the next global outbreak of H1N1 as part of the seasonal influenza in 2013/2014. The widespread occurrence of resistances can manifest itself in a short time span.
The latest data available shows elevated levels of baloxivir resistance in Japan at 4.5% and otherwise little reason for concern. But this may change quickly. Weekly CDC seasonal influenza data including resistance mutations can be found here.
However, investigations into such associations for dual I223V/S247N mutations have not been reported. Therefore, in this study, we assessed the susceptibility of a strain with dual I223V/S247N mutation (HKU-231217-085) to neuraminidase inhibitors using a chemiluminescent neuraminidase inhibition assay. The IC50 value for HKU-231217-085 was 10·63-fold higher (from 0·429 nM to 4·563 nM) against oseltamivir and 3·38-fold higher (from 0·924 nM to 3·120 nM) against zanamivir than the average IC50 value for the three A(H1N1) strains (HKU-231217-099/2023, HKU-231217-100/2023, and 415742/2009) without the dual mutation.